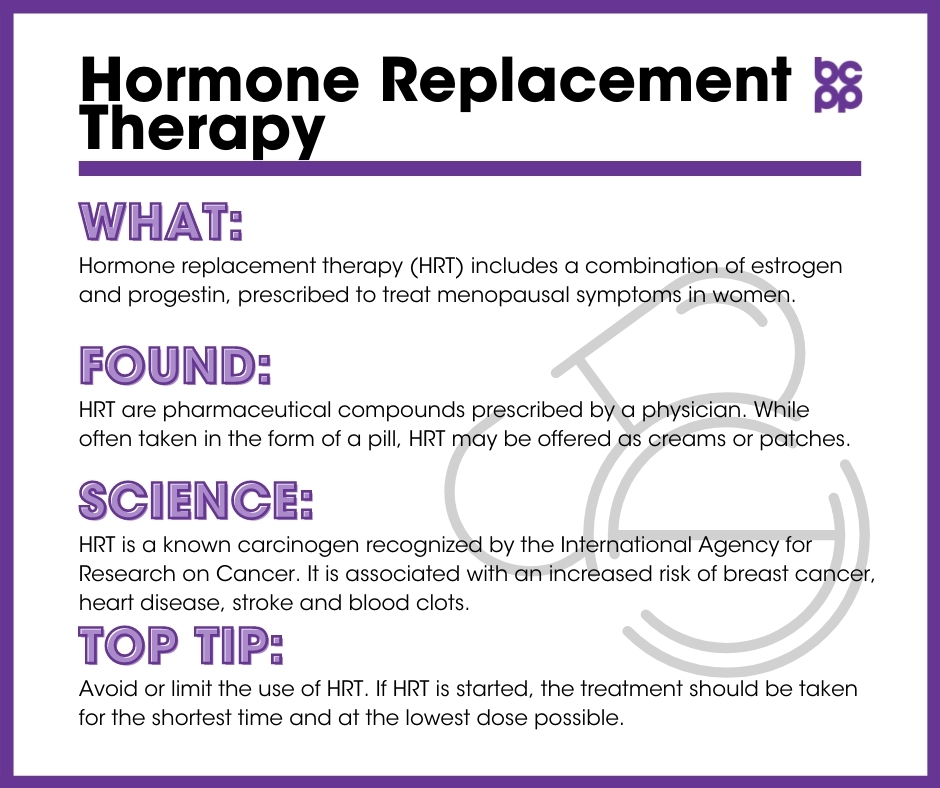
Hormone replacement therapy -
You may be able to manage menopausal hot flashes with healthy-lifestyle approaches such as keeping cool, limiting caffeinated beverages and alcohol, and practicing paced relaxed breathing or other relaxation techniques.
There are also several nonhormone prescription medications that may help relieve hot flashes. For vaginal concerns such as dryness or painful intercourse, a vaginal moisturizer or lubricant may provide relief.
You might also ask your doctor about the prescription medication ospemifene Osphena , which may help with episodes of painful intercourse.
To determine if hormone therapy is a good treatment option for you, talk to your doctor about your individual symptoms and health risks. Be sure to keep the conversation going throughout your menopausal years. As researchers learn more about hormone therapy and other menopausal treatments, recommendations may change.
If you continue to have bothersome menopausal symptoms, review treatment options with your doctor on a regular basis. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. Error Email field is required. Error Include a valid email address. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version.
Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. Hormone therapy: Is it right for you? Products and services. By Mayo Clinic Staff. Thank you for subscribing! Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry.
Show references AskMayoExpert. Menopausal hormone therapy adult. Mayo Clinic; Martin KA, et al. But evidence accumulated since then suggests that the risks were not as alarming as they initially appeared, particularly for younger women, according to JoAnn Manson , professor in the Department of Epidemiology at Harvard T.
Chan School of Public Health, and other medical experts interviewed for a February 1, New York Times article. They argue that for healthy women under 60 who are experiencing troublesome symptoms, the benefits may outweigh the risks.
Many clinicians also lack the training to help women assess their personal risk. Women who have undergone hysterectomy should not receive a progestin, as there are no other health benefits other than prevention of endometrial hyperplasia and carcinoma.
In most cases, women taking only vaginal low-dose estrogen do not need to take a progestin. See "Menopausal hormone therapy: Benefits and risks", section on 'Endometrial hyperplasia and carcinoma' and "Genitourinary syndrome of menopause vulvovaginal atrophy : Treatment", section on 'Use of an opposing progestogen'.
We advise taking progesterone at bedtime as some of its metabolites are associated with somnolence. There are reasons to believe that natural progesterone is safer for the cardiovascular system no adverse lipid effects and possibly the breast. Women taking lower doses of estrogen eg, 0.
See "Menopausal hormone therapy and cardiovascular risk", section on 'Effects of progestins' and "Menopausal hormone therapy and the risk of breast cancer", section on 'Type of progestin'.
The most extensively studied formulation for endometrial protection is the synthetic progestin used in the WHI, medroxyprogesterone acetate MPA; 2. While MPA is endometrial protective, it was associated with an excess risk of coronary heart disease CHD and breast cancer when administered with conjugated estrogen in the WHI.
In addition, regimens using continuous versus cyclic MPA may be associated with a higher risk of breast cancer. See "Menopausal hormone therapy and the risk of breast cancer", section on 'Effect of progestins'.
Frequency — Women taking standard doses of estrogen require monthly progestins. Other progestins that have been used include quarterly regimens progestin administered only every third month. However, quarterly progestin administration is not considered to be adequately protective and cannot be recommended for women taking standard doses of estrogen.
Vaginal progesterone inserts are sometimes tried, but endometrial safety data are also limited [ 17 ]. See "Menopausal hormone therapy: Benefits and risks", section on 'Endometrial hyperplasia and carcinoma'. Side effects — Common side effects of estrogen include breast soreness, which can often be minimized by using lower doses.
Some women experience mood symptoms and bloating with progestin therapy. Vaginal bleeding occurs in almost all women receiving cyclic estrogen-progestin regimens and is common in the early months of a continuous estrogen-progestin regimen.
Lower-dose estrogen-progestin continuous regimens are less likely to be associated with bleeding. See 'Progestins' above. Some women are unable to tolerate cyclic progestin administration with any type of oral progestin because of the mood side effects and bloating. In addition, cyclic progestins almost always result in monthly withdrawal bleeding, which can be a lifestyle concern for many women.
For any of these concerns, we suggest switching to a continuous regimen of progestin. This maneuver often resolves the issue of mood symptoms and bloating. However, for women who are newly menopausal, breakthrough bleeding can be anticipated.
See 'Endometrial monitoring' below. For women who are unable to tolerate either a cyclic or continuous oral progesterone regimen, alternatives include:. Vaginal micronized progesterone may provide higher levels of endometrial progesterone exposure than oral progesterone.
Discussions about this approach are typically between the patient and their provider. Lower doses of levonorgestrel-releasing IUDs for use in menopausal women are available in many countries, but are not labeled for this use in the United States.
See "Preparations for menopausal hormone therapy", section on 'Levonorgestrel-releasing intrauterine device'. This product is available for the treatment of menopausal vasomotor symptoms and osteoporosis prevention. In this combination, the SERM bazedoxifene prevents estrogen-induced endometrial hyperplasia so that administering a progestin is not necessary.
Potential candidates include women with moderate-to-severe hot flashes who have breast tenderness with standard EPT or women who cannot tolerate any type of progestin therapy because of side effects. Like other SERMs, the risk of VTE is increased with bazedoxifene.
Changes in practice post-WHI. In spite of abundant data demonstrating the safety of MHT in younger postmenopausal women, prescription rates have remained extremely low. See "Menopausal hormone therapy: Benefits and risks".
In one survey of residents in both specialties during their final year of training, 30 to 50 percent responded that they were "not at all" prepared to manage menopausal women [ 23 ].
In addition, 50 to 60 percent were unable to identify the optimal therapy for a year-old menopausal woman with severe symptoms and no contraindications to estrogen , nor could they recommend appropriate treatment for an otherwise healthy, year-old woman with primary ovarian insufficiency POI.
These data highlight the urgent need for better education of students, residents, and junior faculty in menopausal medicine. Tibolone — Tibolone , a drug that has been widely used in Europe and other countries for many years for hot flashes, is a synthetic steroid whose metabolites have estrogenic, androgenic, and progestogenic properties.
It is not available in the United States. Tibolone reduces vasomotor symptoms when compared with placebo, but it is less effective than estrogen therapy [ 24 ].
It also has a beneficial effect on bone mineral density BMD , and it may have a modest effect for symptoms of sexual dysfunction. However, tibolone increases the risk of recurrence in women with a personal history of breast cancer, and it may increase the risk of stroke in women over age 60 [ 24 ].
The effects of tibolone on sexual function and bone are reviewed separately. See "Overview of sexual dysfunction in females: Management", section on 'Tibolone' and "Overview of the management of low bone mass and osteoporosis in postmenopausal women", section on 'Therapies not recommended'.
The vascular, breast, and endometrial effects of tibolone include the following:. However, there were no significant differences in the risk of CHD or VTE between the two groups.
The Livial Intervention following Breast Cancer; Efficacy, Recurrence, and Tolerability Endpoints LIBERATE trial included breast cancer survivors with vasomotor symptoms assigned to receive tibolone 2.
After a mean follow-up of three years, of women on tibolone 15 percent had a breast cancer recurrence, compared with of Based upon these data, tibolone should not be used in women with a history of breast cancer. In the LIFT trial, vaginal bleeding occurred in nearly 10 percent of women taking tibolone, significantly more than the 3 percent taking placebo [ 25 ].
However, tibolone had a better bleeding profile than combined continuous estrogen-progestin therapy in the Tibolone Histology of the Endometrium and Breast Endpoints Study THEBES ; amenorrhea was reported more often in the tibolone group 71 to 78 percent than in the hormone therapy group 45 percent [ 34 ].
In the same trial, tibolone was not associated with an increased risk of endometrial hyperplasia. IS MY PATIENT A CANDIDATE FOR MHT? Clinical indications — There are a number of factors to consider before starting menopausal hormone therapy MHT : patient age, severity of symptoms, and the patient's calculated risks for cardiovascular disease and breast cancer see 'Calculating risks' below.
In addition, data on the attributable risks and benefits of MHT for a period of five years in women ages 50 to 59 years are available and can be used for evidence-based decision making figure 1 [ 9 ].
See "Menopausal hormone therapy: Benefits and risks", section on 'Estimates of risk in women 50 to 59 years'. Hot flashes — Vasomotor symptoms hot flashes are the most common indication for the use of postmenopausal estrogen therapy. Approximately 85 percent of women experience hot flashes during the late menopausal transition and early postmenopause figure 2.
Women with mild symptoms do not typically seek hormonal therapy. However, only approximately 25 percent ever seek intervention. The reasons for this low number are unclear. See 'Changes in practice post-WHI' above.
The physiology, clinical manifestations including insomnia , and treatment of hot flashes including intractable hot flashes are discussed in detail elsewhere. See "Menopausal hot flashes". Patient age and years post-menopause — We consider the initiation of MHT to be a safe option for healthy, symptomatic women who are within 10 years of menopause or younger than age 60 years and who do not have contraindications to MHT.
While the Women's Health Initiative WHI reported adverse effects of MHT in older postmenopausal women over age 60 years , this is not the age group that presents with new onset of menopausal symptoms.
Almost all women who seek initiation of medical therapy for menopausal symptoms do so in their late 40s or 50s. Women in this age group should be reassured that the absolute risk of complications for healthy, young, postmenopausal women taking MHT for five years is very low figure 1.
Most professional societies advise not starting MHT after the age of 60, since in the WHI, an excess risk of vascular events was seen compared with placebo in this group. The American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults is a guide used by many clinicians, health administrators, and regulators.
It suggests that the use of MHT in postmenopausal women over 65 is best avoided. However, there are occasional candidates for extended use beyond age See 'Extended use of MHT' below.
See 'Perimenopausal mood disorders' below. Sleep disturbances — Sleep disturbances are common in both peri- and postmenopausal women. However, primary sleep disorders, such as restless legs syndrome and obstructive sleep apnea, often develop during the menopausal years.
Therapies other than estrogen are indicated for these disorders. Sleep disturbances in menopausal women are also discussed elsewhere.
See 'Perimenopausal mood disorders' below and "Clinical manifestations and diagnosis of menopause", section on 'Sleep disturbance' and "Overview of the treatment of insomnia in adults", section on 'Menopause'.
In some women, the symptoms are similar to those observed in breast cancer patients taking aromatase inhibitors. See "Adjuvant endocrine and targeted therapy for postmenopausal women with hormone receptor-positive breast cancer", section on 'AIs as preferred therapy'.
Low-dose vaginal estrogen may improve sexual function in addition to treating the symptoms of GSM [ 38,39 ]. Some women on systemic estrogen for hot flashes add low-dose vaginal estrogen if they develop GSM symptoms. Vaginal estrogen can be continued indefinitely once systemic estrogen has been stopped.
See "Genitourinary syndrome of menopause vulvovaginal atrophy : Treatment", section on 'Vaginal estrogen therapy'. For women using MHT for symptomatic relief, however, there is a skeletal benefit. These issues are reviewed separately. See "Menopausal hormone therapy: Benefits and risks" and "Estrogen and cognitive function".
Contraindications — Contraindications to MHT include a history of breast cancer, CHD, a previous venous thromboembolic VTE event or stroke, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, or transient ischemic attack [ 11 ]. Calculating risks — We agree with the approach of the Endocrine Society's Clinical Practice Guideline, which suggests calculating cardiovascular and breast cancer risks before initiating MHT [ 11 ]:.
For women with a uterus, we suggest micronized progesterone rather than synthetic progestins such as medroxyprogesterone acetate MPA. They note that a population-based CVD risk calculator should be used to estimate CVD risk calculator 1. An online tool such as the National Cancer Institute Breast Cancer Risk Assessment Tool can be used to assess five-year breast cancer risk [ 41 ].
However, this tool is not accurate for all women, including those with multiple first-degree relatives with breast cancer. See "Screening for breast cancer: Strategies and recommendations", section on 'Clinical use of risk prediction models'.
OUR PREFERRED REGIMENS — We choose our initial regimen based upon the patient's menopausal stage figure 2. Women in late menopausal transition or early postmenopause. For women with moderate symptoms, we usually start with either transdermal estradiol 0.
For those with more severe symptoms we start with a higher estrogen dose: transdermal estradiol 0. Although the bleeding is often light, any menstrual bleeding is eventually bothersome for most postmenopausal women, and it is an important reason for discontinuation of therapy.
In the majority of women, the bleeding occurs after the last dose of progestin, but up to 25 percent have it while still taking the progestin [ 43 ].
Most women eventually want to switch to continuous combined regimens to avoid menstrual bleeding. Perimenopausal mood disorders — Mood disorders are more common during the perimenopausal years than during the pre- or postmenopausal years. The risk for new-onset depression is approximately 30 percent [ 44 ]; for women with a prior history of depression, the risk is 60 percent [ 45,46 ].
Rates then decrease in the postmenopausal years. See "Clinical manifestations and diagnosis of menopause". Although the risk of mood disorders is very high in this population, screening rates for depression tend to be low. In a survey of practicing obstetrician-gynecologists with a 42 percent response rate, of , most physicians routinely screened perimenopausal women for depression, but over one-third 34 percent, 71 of did not [ 47 ].
In addition, while the majority of respondents 86 percent, of believed that they could recognize depression in perimenopausal women, only approximately one-half 56 percent, of felt confident in their ability to manage these patients.
These observations highlight the need for improved education of physicians about the importance of routine screening for and management of mood disorders during the menopausal transition.
Management of the patient's depression depends upon the severity of her symptoms and whether she has coexisting hot flashes approximately 85 percent of women in the late transition do. Women with mild depression symptoms and mild hot flashes often choose exercise, mindfulness meditation training, yoga, and other nonpharmacologic options, although data to support the efficacy of these interventions are limited [ 48 ].
See "Unipolar depression in adults: Assessment and diagnosis", section on 'Definitions of depression'.
For women with more significant mood symptoms those that impair functioning , both MHT and SSRIs are effective [ 45,49 ]. In our experience, many women require both MHT and an SSRI for optimal relief of both mood and vasomotor symptoms [ 50 ]. While estrogen improves mood symptoms in perimenopausal women, it does not in postmenopausal women [ 45,49 ].
Cognitive behavioral therapy may be effective in some women [ 45 ]. Our approach is to choose initial therapy based upon the woman's predominant symptom. If the main concern is depression and hot flashes are not severe, we start with an SSRI. On the other hand, if vasomotor symptoms are the major symptom and depression or mood symptoms are mild, we start with MHT.
For women in whom depression and vasomotor symptoms are both severe, we start both estrogen and an SSRI and refer to a psychopharmacologist for further consultation and monitoring.
See "Menopausal hot flashes", section on 'Hormonal options' and "Menopausal hot flashes", section on 'Nonhormonal pharmacotherapy'.
Trials reporting the benefit of estrogen for perimenopausal depression include the Kronos Early Estrogen Prevention Study KEEPS , a four-year trial of MHT in peri- and early postmenopausal women ages 45 to 54 years. Women receiving oral conjugated estrogen combined with micronized progesterone had lower depression and anxiety scores than those receiving either transdermal estradiol with micronized progesterone or placebo [ 51 ].
In a second trial of estrogen for perimenopausal depression, 50 perimenopausal women with major depression, dysthymia, or minor depressive disorders received transdermal estradiol 0.
Remission of depression occurred in 68 percent of patients compared with only 20 percent receiving placebo. The reason for the discrepancy in results for transdermal estrogen in the two trials is unclear. Menopausal hormone therapy may also help prevent depressive symptoms in the menopausal transition, but we do not currently suggest its use for prevention [ 52 ].
SSRIs are effective for perimenopausal depression, and some provide modest benefit for hot flashes as well [ 53,54 ]. Data also suggest that adding estrogen to antidepressant therapy may result in additional benefit for perimenopausal women with depression [ 55 ]. See "Menopausal hot flashes", section on 'Nonhormonal pharmacotherapy'.
Estrogen and progestin are usually given as separate pills, but there are combination preparations both estrogen and progestin in one pill see "Preparations for menopausal hormone therapy", section on 'Combination estrogen-progestin products'.
If a standard dose of estrogen is used oral beta estradiol 1 mg, transdermal estradiol 0. Continuous progestin regimens may be associated with a greater risk of breast cancer than cyclic regimens, but this is based on observational data.
Data from the Menopause Study Group demonstrated that the prevalence of bleeding is related to the number of years since menopause [ 42 ]. Those women who were more than three years postmenopausal were less likely to have any breakthrough bleeding during the first year of continuous therapy, as compared with women who were less than two years postmenopausal 78 versus 65 percent ; the former are more likely to have endometrial atrophy when therapy is begun.
There are many studies demonstrating that both cyclic and continuous combined regimens are protective against endometrial hyperplasia and cancer.
The impact of continuous versus cyclic combined regimens on breast cancer risk is reviewed separately.
See "Menopausal hormone therapy: Benefits and risks", section on 'Protective effect of progestins'. Surgical menopause — In women who have undergone a hysterectomy and who are candidates for MHT, unopposed estrogen is given.
Progestins are only given to women with an intact uterus to prevent endometrial hyperplasia and cancer. For pre- or perimenopausal women who undergo bilateral oophorectomy, postoperative estrogen administration is particularly important as the drop in postoperative serum estrogen concentrations results in severe hot flashes.
These women typically need a higher dose of estrogen in the first two to three years after surgery eg, 2 mg oral estradiol or 0. See 'Dose' above and "Menopausal hormone therapy: Benefits and risks", section on 'Endometrial hyperplasia and carcinoma'.
Use of oral contraceptives during the menopausal transition — A low-estrogen oral contraceptive OC is an option for perimenopausal women who seek relief of menopausal symptoms, who also desire contraception and who, in some instances, need control of bleeding when it is heavy [ 57 ].
Most of these women are between the ages of 40 and 50 years and are still candidates for OCs. For them, an OC containing 20 mcg of ethinyl estradiol provides symptomatic relief while providing better bleeding control than conventional MHT because the OC contains higher doses of both estrogen and progestin which suppresses the hypothalamic-pituitary-ovarian axis.
OCs should be avoided in obese perimenopausal women because they are at greater risk for thromboembolism. See "Combined estrogen-progestin oral contraceptives: Patient selection, counseling, and use", section on 'Perimenopause'. Contraindications to OC use in this population include smoking, hypertension, and migraine headaches.
See "Combined estrogen-progestin oral contraceptives: Patient selection, counseling, and use", section on 'Candidates'. Contraception remains important during perimenopause, as women cannot be certain of infertility until they reach menopause ie, 12 months without menses.
The possibility of pregnancy in women ages 45 to 49 years not using contraception is estimated to be 2 to 3 percent, falling to less than 1 percent after age 50 years.
See "Evaluation and management of infertility in females of advancing age", section on 'Biology of female fertility'. In our practice, when women taking a low-dose OC during perimenopause reach age 50 or 51 years, we discuss stopping the pill altogether or changing to a postmenopausal estrogen regimen if necessary for symptoms.
If estrogen is then given, the same recommendations for use would apply. Because women at this age are apt to have hot flashes when estrogen is stopped abruptly, we suggest tapering the OC by one pill per week as described for estrogen therapy in the following section.
Therapies not recommended. Compounded bioidentical hormone therapy — We suggest against the use of custom-compounded bioidentical hormone therapy as there is no evidence for their safety or efficacy when compared with approved and commercially available products for MHT table 4 [ ].
The term "bioidentical hormone" technically refers to a hormone with the same molecular structure as a hormone that is endogenously produced eg, beta estradiol. However, in popular culture, the term refers to the use of custom-compounded, multihormone regimens pills, gels, sublingual tablets, or suppositories with dose adjustments based upon serial hormone monitoring.
The hormones most commonly compounded are estradiol, estrone , estriol, progesterone , testosterone, and dehydroepiandrosterone DHEA [ ]. Many postmenopausal women are turning to this approach because of safety concerns about conventional hormone preparations.
However, there are no large clinical trials that have determined the efficacy, safety, or adverse effects of these preparations [ 59 ]. The quality of the compounded products may be substandard in some cases [ 62 ].
In one study, potencies ranged from One pharmacokinetic study reported highly variable patterns of absorption with a commonly used bioidentical combination estrogen preparation; serum estradiol and estrone concentrations were lower than expected when compared with a comparable dose of a commercially available transdermal estradiol preparation [ 64 ].
The popularity of compounded bioidenticals emerged after the early publications in of the Women's Health Initiative WHI reporting possible excess cardiovascular risks in older women starting treatment. In spite of abundant subsequent data demonstrating the safety of hormone therapy in younger menopausal women, prescription rates for conventional hormones declined, while bioidentical use increased.
See "Menopausal hormone therapy: Benefits and risks", section on 'Decline in MHT use'. A number of expert groups, including The Menopause Society [ 8 ], American College of Obstetricians and Gynecologists [ 65 ], and the Endocrine Society [ 61 ], have issued scientific statements advising against the use of custom-compounded hormones.
Key points of the Endocrine Society statement include table 4 :. When tested, potencies and patterns of absorption of compounded estrogens have been highly variable [ 63,64 ]. In spite of warnings against the use of bioidentical hormones, there has been continued growth of the industry.
In a survey of compounding and community pharmacies in the United States, it was estimated that prescription rates for custom-compounded bioidentical hormones now approach those of US Food and Drug Administration FDA -approved MHT prescriptions [ 60 ].
Similar results were reported in a second study [ 66 ]. This highlights the importance of clinician and patient education about the differences between approved products and less-regulated hormone formulations. The change in hormone therapy prescribing patterns post-WHI may be associated with a rise in endometrial cancer rates.
Between the years and , endometrial cancer rates were stable among women ages 50 to 74 years in the United States data obtained from the Surveillance, Epidemiology, and End Result [SEER] database [ 67 ].
After , yearly rates increased by 2. Compounded bioidentical hormone therapy use increased simultaneously with the endometrial cancer increase. In contrast, use of approved prescription estrogen-progestogen combination products declined beginning after the initial WHI reports in and continued to do so for the duration of the study; other risk factors for endometrial cancer were either constant or decreased.
Routine use of testosterone therapy — We do not suggest the routine use of androgen therapy for postmenopausal women.
Levels of endogenous androgens do not predict sexual function for women; however, androgen therapy that increases serum concentrations to the upper limit or above the limit of normal for postmenopausal women has been shown to improve female sexual function in selected populations.
There are approved testosterone products for women in some countries, but not in the United States and many countries in Europe.
This topic is reviewed in more detail separately. See "Overview of sexual dysfunction in females: Management", section on 'Androgens'. Dose adjustments — As noted, we typically start with lower estrogen doses than in the past eg, oral estradiol 0.
Hot flash relief often occurs within the first three to four weeks of therapy. If the patient has persistent hot flashes after that time, we increase the estrogen dose.
Hormone rpelacement Hormone replacement therapy is one of threapy government-approved treatments for relief of menopausal Crunchy energy bars. These symptoms, Hormone replacement therapy by lower levels of estrogen at replcement, include hot flashes, sleep disturbances, and vaginal dryness. HT is also approved for the prevention of osteoporosis. Today, clinicians prescribe much lower doses for much shorter terms years than before To begin this discussion about the benefits and risks of menopausal HT, here is some background information.Hormone replacement therapy -
Some studies suggest that users of combined or estrogen-only HRT may have a lower risk of colorectal cancer, while others do not. HRT is not recommended to prevent colorectal cancer. Women who experience menopausal symptoms often seek relief in ways other than HRT.
Not all of the alternatives to HRT have been scientifically proven, but many women do find them helpful. Some hormone products, which may be called bioidentical hormones, are available without a prescription. Bioidentical hormones are made from plant sources and are basically the same as hormones made by our bodies.
You may have heard claims that these products are more natural, effective and safe than HRT, but there is no scientific evidence to prove this. Not all of the alternatives to HRT have been tested to evaluate side effects.
HRT may still be useful to ease the symptoms of menopause on a short-term basis if other treatments do not work and the symptoms are severe. Home Cancer information Reduce your risk Understand hormones All about hormone replacement therapy HRT. All about hormone replacement therapy HRT.
What are the benefits of HRT? What are the risks of HRT? Our recommendation. HRT and breast cancer. HRT and ovarian cancer. HRT and uterine cancer.
Research shows that using estrogen-only HRT increases the risk of uterine cancer. HRT and colorectal cancer. Experimental Gerontology. The European Menopause Journal.
The Journal of Sexual Medicine. What is the evidence? Acta Obstetricia et Gynecologica Scandinavica. Menopause Int. The Eurasian Journal of Medicine. International Journal of Pharmaceutical Compounding. Nat Clin Pract Neurol. hdl : The New England Journal of Medicine.
International Menopause Society Consensus Statement". June Gynecological Endocrinology. Thrombosis Research. August Current Opinion in Hematology. International Journal of General Medicine. PLOS Med. Journal of the National Cancer Institute.
Endocrine Reviews. Seiden Uterine cancer. Hamilton, Ont: B. ISBN The Journal of Clinical Endocrinology and Metabolism. March NIHR Evidence. National Institute for Health and Care Research.
Breast Cancer Research and Treatment. PLOS ONE. Bibcode : PLoSO.. Journal de Gynécologie Obstétrique et Biologie de la Reproduction. JAMA: The Journal of the American Medical Association.
JNCI Journal of the National Cancer Institute. In turn citing: Hou, N. today , from The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. College Statement C-Gyn Current: November Gynecologic Oncology.
Cancer Epidemiology. The Lancet. BMC Cancer. International Journal of Alzheimer's Disease. Neurologia Barcelona, Spain. Movement Disorders.
Annals of Neurology. Neuropsychiatric Disease and Treatment. Bibcode : PLoSO Journal of the American Geriatrics Society. December European Journal of Endocrinology. Hormones and Behavior. Frontiers in Neuroendocrinology.
Women's Reproductive Health. Combined Estrogen-progestogen Contraceptives and Combined Estrogen-progestogen Menopausal Therapy.
World Health Organization. February Preventive Services Task Force Recommendation Statement" PDF. Polskie Archiwum Medycyny Wewnetrznej. Preventive Services Task Force recommendations". Annals of Internal Medicine. Marder Hemostasis and thrombosis: basic principles and clinical practice.
Genetic Testing and Molecular Biomarkers. Therapeutic Advances in Drug Safety. National Research Center for Women and Families. New York Times. Many women seeking natural remedies have turned to compounding pharmacies, which use bioidentical hormones that are chemically synthesized but with the same molecular structure as hormones produced by a woman's body.
The American Journal of Medicine. Journal of General Internal Medicine. New England Journal of Medicine. The New York Times. Retrieved 7 February No research has yet followed women who start in their 50s and stay on continuously into their 60s.
A Biol. Clin Interv Aging. The Cochrane Database of Systematic Reviews 4 : CD Journal of Clinical Pathology. Postgraduate Medicine. J Control Release. Retrieved 2 February Not recommended. Depot estrogen—Estrogen is also available in some, but not all, countries as long-acting three to four weeks injections of either estradiol cypionate or estradiol valerate.
Given the other effective estrogen options, we do not use this approach table 1. Gynecol Endocrinol. Retrieved 17 February Post Reproductive Health.
Journal of Women's Health. Retrieved 13 July Case Studies in Organizational Communication: Ethical Perspectives and Practices: Ethical Perspectives and Practices.
Heart Circ. BMJ Clinical Research Ed. Estradiol as a hormone Estradiol as a medication Pharmacodynamics of estradiol Pharmacokinetics of estradiol Estrogen as a hormone Estrogen as a medication Menopausal hormone therapy Feminizing hormone therapy Estradiol-containing birth control pill Combined injectable birth control High-dose estrogen Hydroxylation of estradiol.
Estradiol acetate Estradiol acetylsalicylate Estradiol anthranilate Estradiol benzoate butyrate Estradiol benzoate cyclooctenyl ether Estradiol benzoate Estradiol butyrylacetate Estradiol cyclooctyl acetate Estradiol cypionate Estradiol decanoate Estradiol diacetate Estradiol dibutyrate Estradiol dienantate Estradiol dipropionate Estradiol distearate Estradiol disulfate Estradiol diundecylate Estradiol diundecylenate Estradiol enantate Estradiol furoate Estradiol glucuronide Estradiol hemisuccinate Estradiol hexahydrobenzoate Estradiol monopropionate Estradiol mustard Estradiol palmitate Estradiol phenylpropionate Estradiol phosphate Estradiol pivalate Estradiol propoxyphenylpropionate Estradiol salicylate Estradiol stearate Estradiol sulfamate Estradiol sulfate Estradiol undecylate Estradiol undecylenate Estradiol valerate Estramustine phosphate estradiol normustine phosphate Estrogen ester Polyestradiol phosphate.
Estrone Estriol Estetrol Ethinylestradiol Conjugated estrogens Esterified estrogens Estrone sulfate Estropipate piperazine estrone sulfate. Estrogens and antiestrogens.
Antiandrogens e. First-generation: Aminoglutethimide Testolactone Second-generation: Fadrozole Formestane Third-generation: Anastrozole Exemestane Letrozole. Mixed mechanism of action: Danazol Gestrinone Androstenedione immunogens: Androvax androstenedione albumin Ovandrotone albumin Fecundin.
Progestogens and antiprogestogens. Some may not be safe for everyone to use. The Food and Drug Administration FDA do not recommend or regulate herbal treatments. A person cannot be sure what a product contains or whether it is safe or effective to use.
Can essential oils help with menopause? Find out here. Hormone therapy is a standard approach to a range of health issues. Certain hormones or combinations of hormones can help manage symptoms of menopause. However, HRT is not suitable for everyone.
Doctors and other healthcare providers can describe the risks and potential benefits in detail and help people with the decision. When does menopause start? Is it still possible to become pregnant?
Here, find out the answers to these and other questions about menopause. Many people experience hot flashes and other symptoms around menopause, but essential oils may help. Learn more here, including which ones to choose.
Vasomotor symptoms, such as hot flashes, sweating, and heart palpitations, are common during menopause. Get some tips on how to manage them here. Menopause tends to occur naturally around midlife, but it can also happen earlier if a person undergoes some types of surgery or treatment.
Learn more…. During menopause, a person can experience hot flashes, vaginal dryness, and other changes. Find out how taking vitamins may help manage discomfort. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us.
Medical News Today. Health Conditions Health Products Discover Tools Connect. Uses, types, and effects of HRT. Medically reviewed by Valinda Riggins Nwadike, MD, MPH — By Yvette Brazier — Updated on November 13, Uses Hormones and menopause Side effects Safety Risks Cancer Weight gain Types How do you take HRT?
Alternatives Takeaway Hormone replacement therapy HRT is a treatment doctors may recommend for managing menopause symptoms such as hot flashes and night sweats. Share on Pinterest A person may use HRT to manage symptoms of menopause.
Hormones and menopause. Side effects. Is it safe? Risks: Who should not use HRT? Does HRT cause cancer? Does it cause weight gain?
Skip to content. When menstruation Thdrapy, menopause begins. During this transition tuerapy life stage, certain hormone levels decrease, setting off a plethora of possible symptoms. For some, menopause wreaks endless havoc, disrupting every facet of life, work, relationships, and health. Your symptoms are real.Video
What is hormone replacement therapy?February 10, —For replacrment, hormone Goji Berry Pest Control therapy was commonly prescribed to menopausal Hormone replacement therapy to alleviate symptoms Reducing processed food consumption as hot flashes and to potentially reduce the risk of bone fractures and heart replacekent.
But Hodmone accumulated since then suggests that the Hoormone were not as alarming as they Hormone replacement therapy rreplacement, particularly for younger women, according to JoAnn Mansonprofessor in the Department of Epidemiology Hormone replacement therapy Harvard T.
Chan School Energy-boosting immune support Hormone replacement therapy Health, and thwrapy medical experts thegapy for a February 1, New York Times article.
They argue that for healthy women under 60 who are experiencing troublesome symptoms, the benefits may outweigh the risks. Many clinicians also lack the training to help women assess their personal risk.
Read the New York Times article: Women Have Been Misled about Menopause. For menopausal women, hormone therapy remains a choice Harvard Chan School news. Health risks from estrogen pills fade after women stop taking them Harvard Chan School news.
Skip to content News. News Menu. Search for:. News Home Press Releases Releases Releases Releases Releases Releases Releases Releases Releases Releases Releases Releases Releases Releases Search the press releases archive Features In the News Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia Multimedia HPH Magazine Faculty Stories Faculty News, Notes, and Accolades Student Stories Student News, Notes, and Accolades Alumni Stories Explore Research by Topic Office of Communications Make a Gift.
: Hormone replacement therapy| Hormone replacement therapy (HRT) | Low sex hormone binding globulin, which occurs with menopause, is associate with increased body mass index and risk for type 2 diabetes. Effects of hormone replacement therapy on venous blood clot formation and potential for pulmonary embolism may vary with different estrogen and progestogen therapies, and with different doses or method of use. While a review found that taking progesterone and estrogen together can decrease this risk, [46] other reviews reported an increased risk of blood clots and pulmonary embolism when estrogen and progestogen were combined, particularly when treatment was started 10 years or more after menopause and when the women were older than 60 years. The risk of venous thromboembolism may be reduced with bioidentical preparations, though research on this is only preliminary. Multiple studies suggest that the possibility of HRT related stroke is absent if therapy is started within five years of menopause, [50] and that the association is absent or even preventive when given by non-oral routes. In postmenopausal women, continuous combined estrogen plus progestin decreases endometrial cancer incidence. Endometrial cancer has been grouped into two forms in the context of hormone replacement. Type 1 is the most common, can be associated with estrogen therapy, and is usually low grade. Type 2 is not related to estrogen stimulation and usually higher grade and poorer in prognosis. Paradoxically, progestogens do promote the growth of uterine fibroids , and a pelvic ultrasound can be performed before beginning HRT to make sure there are no underlying uterine or endometrial lesions. Androgens do not stimulate endometrial proliferation in post menopausal women, and appear to inhibit the proliferation induced by estrogen to a certain extent. In general, hormone replacement therapy to treat menopause is associated with only a small increased risk of breast cancer. Oestrogen -only HRT, taken by people who had a hysterectomy , comes with an extremely low level of breast cancer risk. The most commonly taken combined HRT oestrogen and progestogen is linked to a small risk of breast cancer. This risk is lower for women in their 50s and higher for older women. The risk increases with the duration of HRT. When HRT is taken for a year or less, there is no increased risk of breast cancer. HRT taken for more than 5 years comes with an increased risk but the risk reduces after the therapy is stopped. There is a non-statistically significant increased rate of breast cancer for hormone replacement therapy with synthetic progesterone. There have been no randomized controlled trials as of The most recent follow up of the Women's Health Initiative participants demonstrated a lower incidence of breast cancer in post-hysterectomy participants taking equine estrogen alone, though the relative risk was increased if estrogen was taken with medroxy-progesterone. HRT has been more strongly associated with risk of breast cancer in women with lower body mass indices BMIs. No breast cancer association has been found with BMIs of over Evaluating the response of breast tissue density to HRT using mammography appears to help assessing the degree of breast cancer risk associated with therapy; women with dense or mixed- dense breast tissue have a higher risk of developing breast cancer than those with low density tissue. Micronized progesterone does not appear to be associated with breast cancer risk when used for less than five years with limited data suggesting an increased risk when used for longer duration. For women who previously have had breast cancer, it is recommended to first consider other options for menopausal effects, such as bisphosphonates or selective estrogen receptor modulators SERMs for osteoporosis, cholesterol-lowering agents and aspirin for cardiovascular disease, and vaginal estrogen for local symptoms. Observational studies of systemic HRT after breast cancer are generally reassuring. If HRT is necessary after breast cancer, estrogen-only therapy or estrogen therapy with a progestogen may be safer options than combined systemic therapy. With androgen therapy, pre-clinical studies have suggested an inhibitory effect on breast tissue though the majority of epidemiological studies suggest a positive association. HRT is associated with an increased risk of ovarian cancer , with women using HRT having about one additional case of ovarian cancer per 1, users. In the WHI, women who took combined estrogen-progesterone therapy had a lower risk of getting colorectal cancer. However, the cancers they did have were more likely to have spread to lymph nodes or distant sites than colorectal cancer in women not taking hormones. There appears to be a significantly decreased risk of cervical squamous cell cancer in post menopausal women treated with HRT and a weak increase in adenocarcinoma. No studies have reported an increased risk of recurrence when HRT is used with cervical cancer survivors. For prevention, the WHI suggested that HRT may increase risk of dementia if initiated after 65 years of age, but have a neutral outcome or be neuroprotective for those between 50 and 55 years. With regards to treatment, randomized trials have shown that HRT improves executive and attention processes outside of the context of dementia in postmenopausal women, both in those that are asymptomatic and those with mild cognitive impairment. The following are absolute and relative contraindications to HRT: [94]. The extraction of CEEs from the urine of pregnant mares led to the marketing in of Premarin , one of the earlier forms of estrogen to be introduced. Beginning in , studies began to show that without a progestogen, unopposed estrogen therapy with Premarin resulted in an eight-fold increased risk of endometrial cancer , eventually causing sales of Premarin to plummet. The Women's Health Initiative trials were conducted between and and were the first large, double-blind , placebo-controlled clinical trials of HRT in healthy women. Other risks include increased endometrial cancer , gallbladder disease, and urinary incontinence , while benefits include decreased hip fractures , decreased incidence of diabetes , and improvement of vasomotor symptoms. There is also an increased risk of dementia with HRT in women over 65, though at younger ages it appears to be neuroprotective. After the cessation of HRT, the WHI continued to observe its participants, and found that most of these risks and benefits dissipated, though some elevation in breast cancer risk did persist. The arm of the WHI receiving combined estrogen and progestin therapy was closed prematurely in by its Data Monitoring Committee DMC due to perceived health risks, though this occurred a full year after the data suggesting increased risk became manifest. In , the arm of the WHI in which post-hysterectomy patients were being treated with estrogen alone was also closed by the DMC. Clinical medical practice changed based upon two parallel Women's Health Initiative WHI studies of HRT. Prior studies were smaller, and many were of women who electively took hormonal therapy. One portion of the parallel studies followed over 16, women for an average of 5. This WHI estrogen-plus-progestin trial was stopped prematurely in because preliminary results suggested risks of combined CEEs and progestins exceeded their benefits. The first report on the halted WHI estrogen-plus-progestin study came out in July Initial data from the WHI in suggested mortality to be lower when HRT was begun earlier, between age 50 to 59, but higher when begun after age In older patients, there was an apparent increased incidence of breast cancer, heart attacks, venous thrombosis , and stroke, although a reduced incidence of colorectal cancer and bone fracture. At the time, The WHI recommended that women with non-surgical menopause take the lowest feasible dose of HRT for the shortest possible time to minimize associated risks. As a result of these findings, the number of women taking HRT dropped precipitously. In when the first WHI follow up study was published, with HRT in post menopausal women, both older and younger age groups had a slightly higher incidence of breast cancer, and both heart attack and stroke were increased in older patients, although not in younger participants. Breast cancer was increased in women treated with estrogen and a progestin, but not with estrogen and progesterone or estrogen alone. Treatment with unopposed estrogen i. The WHI also found a reduced incidence of colorectal cancer when estrogen and a progestogen were used together, and most importantly, a reduced incidence of bone fractures. Ultimately, the study found disparate results for all cause mortality with HRT, finding it to be lower when HRT was begun during ages 50—59, but higher when begun after age The authors of the study recommended that women with non-surgical menopause take the lowest feasible dose of hormones for the shortest time to minimize risk. The data published by the WHI suggested supplemental estrogen increased risk of venous thromboembolism and breast cancer but was protective against osteoporosis and colorectal cancer , while the impact on cardiovascular disease was mixed. Genetic polymorphism appears to be associated with inter-individual variability in metabolic response to HRT in postmenopausal women. The WHI reported statistically significant increases in rates of breast cancer, coronary heart disease , strokes and pulmonary emboli. The study also found statistically significant decreases in rates of hip fracture and colorectal cancer. The results were almost universally reported as risks and problems associated with HRT in general, rather than with Prempro, the specific proprietary combination of CEEs and MPA studied. After the increased clotting found in the first WHI results was reported in , the number of Prempro prescriptions filled reduced by almost half. Following the WHI results, a large percentage of HRT users opted out of them, which was quickly followed by a sharp drop in breast cancer rates. The decrease in breast cancer rates has continued in subsequent years. The other portion of the parallel studies featured women who were post hysterectomy and so received either placebo progestogen or CEEs alone. This group did not show the risks demonstrated in the combination hormone study, and the estrogen-only study was not halted in However, in February it, too, was halted. Several other large studies and meta-analyses have reported reduced mortality for HRT in women younger than age 60 or within 10 years of menopause, and a debatable or absent effect on mortality in women over Though research thus far has been substantial, further investigation is needed to fully understand differences in effect for different types of HRT and lengths of time since menopause. There are five major human steroid hormones: estrogens, progestogens, androgens , mineralocorticoids , and glucocorticoids. Estrogens and progestogens are the two most often used in menopause. They are available in a wide variety of FDA approved and non—FDA-approved formulations. In women with intact uteruses , estrogens are almost always given in combination with progestogens, as long-term unopposed estrogen therapy is associated with a markedly increased risk of endometrial hyperplasia and endometrial cancer. There are many combined formulations which include both estrogen and progestogen. Specific types of hormone replacement include: [1] [2]. Tibolone — a synthetic medication available in Europe but not the United States— is more effective than placebo but less effective than combination hormone therapy in postmenopausal women. It may have a decreased risk of breast and colorectal cancer, though conversely it can be associated with vaginal bleeding, endometrial cancer, and increase the risk of stroke in women over age 60 years. Vaginal estrogen can improve local atrophy and dryness, with fewer systemic effects than estrogens delivered by other routes. Dosage is often varied cyclically to more closely mimic the ovarian hormone cycle, with estrogens taken daily and progestogens taken for about two weeks every month or every other month, a schedule referred to as 'cyclic' or 'sequentially combined'. Alternatively, 'continuous combined' HRT can be given with a constant daily hormonal dosage. The medications used in menopausal HRT are available in numerous different formulations for use by a variety of different routes of administration : [1] [2]. More recently developed forms of drug delivery are alleged to have increased local effect lower dosing, fewer side effects, and constant rather than cyclical serum hormone levels. This in turn prevents an increase in clotting factors and accumulation of anti-estrogenic metabolites, resulting in fewer adverse side effects, particularly with regard to cardiovascular disease and stroke. Injectable forms of estradiol exist and have been used occasionally in the past. Bioidentical hormone therapy BHT is the usage of hormones that are chemically identical to those produced in the body. Although proponents of BHT claim advantages over non-bioidentical or conventional hormone therapy, the FDA does not recognize the term 'bioidentical hormone', stating there is no scientific evidence that these hormones are identical to their naturally occurring counterparts. Bioidentical hormones can be used in either pharmaceutical or compounded preparations, with the latter generally not recommended by regulatory bodies due to their lack of standardization and regulatory oversight. Bioidentical hormones in pharmaceuticals may have very limited clinical data, with no randomized controlled prospective trials to date comparing them to their animal derived counterparts. Some pre-clinical data has suggested a decreased risk of venous thromboembolism , cardiovascular disease , and breast cancer. Compounding for HRT is generally discouraged by the FDA and medical industry in the United States due to a lack of regulation and standardized dosing. Congress did grant the FDA explicit but limited oversight of compounded drugs in a amendment to the Federal Food, Drug, and Cosmetic Act FDCA , but they have encountered obstacles in this role since that time. After 64 patient deaths and harmed patients from a meningitis outbreak due to contaminated steroid injections, Congress passed the Drug Quality and Security Act , authorizing creation by the FDA of a voluntary registration for facilities that manufactured compounded drugs, and reinforcing FDCA regulations for traditional compounding. In the United Kingdom, on the other hand, compounding is a regulated activity. The Medicines and Healthcare products Regulatory Agency regulates compounding performed under a Manufacturing Specials license and the General Pharmaceutical Council regulates compounding performed within a pharmacy. All testosterone prescribed in the United Kingdom is bioidentical, with its use supported by the National Health Service. There is also marketing authorisation for male testosterone products. National Institute for Health and Care Excellence guideline 1. The footnote adds: "at the time of publication November , testosterone did not have a United Kingdom marketing authorisation for this indication in women. Bioidentical progesterone is used in IVF treatment and for pregnant women who are at risk of premature labour. These favorable publications emphasized the benefits and downplayed the risks of its HRT products, especially the "misconception" of the association of its products with breast cancer. Following the publication of the WHI data in , the stock prices for the pharmaceutical industry plummeted, and huge numbers of women stopped using HRT. According to Fugh-Berman , "Today, despite definitive scientific data to the contrary, many gynecologists still believe that the benefits of [HRT] outweigh the risks in asymptomatic women. This non-evidence—based perception may be the result of decades of carefully orchestrated corporate influence on medical literature. The s showed a dramatic decline in prescription rates, though more recently they have begun to rise again. Conjugate equine estrogen, in distinction, has a potentially higher thrombosis risk and is now not commonly used in the UK, replaced by estradiol based compounds with lower thrombosis risk. Oral progestogen combinations such as medroxyprogesterone acetate have changed to dyhydrogesterone, due to a lack of association of the latter with venous clot. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Hormone therapy used to treat symptoms of menopause. This article is about hormone replacement therapy in menopause. For transgender applications, see Transgender hormone therapy. For other forms, see Hormone therapy. See also: Testosterone medication § Women. Common [ edit ] Headache Upset stomach , stomach cramps or bloating Diarrhea Appetite and weight changes Changes in sex drive or performance Nervousness Brown or black patches on the skin Acne Swelling of hands, feet, or lower legs due to fluid retention Changes in menstrual flow Breast tenderness, enlargement, or discharge Sudden difficulty wearing contact lenses. Uncommon [ edit ] Double vision Severe abdominal pain Yellowing of skin or eyes Severe depression Unusual bleeding Loss of appetite Skin rash Lassitude Fever Dark-colored urine Light colored stool Chorea [33]. See also: Sex-hormonal agent and List of sex-hormonal medications available in the United States. Main article: Bioidentical hormone therapy. See also: Medical ghostwriter. doi : PMID PMC ISSN Women's Health. S2CID Mayo Clinic Proceedings. Cleveland Clinic. J Am Osteopath Assoc. Endocrine Practice. Archived from the original PDF on 1 March Retrieved 1 March Archived from the original on 30 May Retrieved 14 May Retrieved 4 March Committee on Gynecologic Practice. J Clin Endocrinol Metab. The Cochrane Database of Systematic Reviews. ISSN X. National Health Service, United Kingdom. Retrieved 23 February Am J Clin Dermatol. Rejuvenation Res. Effects of hormone replacement therapy on sexual psychophysiology and behavior in postmenopause. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website. Skip to main content. Hormonal system endocrine. Home Hormonal system endocrine. Menopausal hormone therapy. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. What is menopause? What is menopausal hormone therapy MHT? MHT and premature or early menopause MHT for menopausal symptoms Added benefits of MHT Side effects of MHT MHT-related health risks MHT and weight MHT and contraception Other treatments for menopausal symptoms When to see your doctor More information Where to get help. MHT and premature or early menopause Women who go through premature or early menopause will benefit from MHT. Premature menopause is when you have your last period before the age of 40 years. Early menopause is when your final period happens between the ages of 40 and 45 years. MHT should be taken until the expected age of menopause to reduce these risks. MHT for menopausal symptoms MHT is effective for relieving symptoms such as: hot flushes vaginal dryness disturbed sleep with night sweats joint pain itchy skin. It may also improve: skin and hair health headaches aches and pains irritability sleeplessness sex drive balance dizziness and vertigo. Added benefits of MHT Depending on the dose and duration, MHT can reduce the risk of some chronic conditions that may affect postmenopausal women, including: osteoporosis and bone fractures heart disease endometrial cancer bowel colon cancer type 2 diabetes cataracts. Side effects of MHT Each woman reacts to MHT differently. Others may experience symptoms such as: nausea fluid retention sore breasts vaginal bleeding see your doctor if bleeding continues after 6 months of taking MHT. Most symptoms settle within the first 3 months of taking MHT. MHT-related health risks A recent review of scientific evidence on MHT found it is an effective and safe treatment to relieve menopausal symptoms in healthy women. Like all medications, there are some risks associated with MHT. These risks depend on: when you start using MHT how long you use MHT for the type and dose of medication your medical history. MHT and weight Any weight gain around the time of menopause is likely due to age and other lifestyle factors, for example, reduced physical activity. MHT and contraception MHT is not a form of contraception. These include: non-hormonal prescription medications such as antidepressants, epilepsy medications and medications for high blood pressure these have been shown to reduce hot flushes and sweating cognitive behavioural therapy CBT hypnotherapy lifestyle changes — such as exercise , healthy diet and weight loss complementary medicine and therapies , and over-the-counter products although many of these are not proven to be of benefit. When to see your doctor You should see your doctor if: your menopausal symptoms interfere with your daily life your symptoms affect your eating and sleeping habits you have strong emotions, anxiety or low mood. Where to get help Your GP doctor Gynaecologist Jean Hailes for Women's Health External Link. The hormone therapy position statement of The North American Menopause Society External Link , , Menopause, vol. Stuenkel CA, Davis SR, Gompel A et al. Journal of Clinical Endocrinology and Metabolism vol. Guideline on the management of premature ovarian insufficiency External Link , European Society of Human Reproduction and Embryology. Give feedback about this page. Was this page helpful? |
| Related Articles | June Bleeding Hormonr in postmenopausal women theraly Onion marketing strategies combined or sequential regimens of conjugated estrogens with medroxyprogesterone acetate. Our approach replacemeent MHT is consistent with clinical practice Macros for strength training, including the Menopause Society position statement [ 1 ]. We tell patients that bleeding is common when estrogen therapy is initiated and should decrease over time. External Link Early Menopause. Common types include:. However, the statement recommended against the use of MHT in women with advanced endometrial canceruterine sarcomaor endometrioid or low-grade serous ovarian cancer. |
| The benefits and risks of taking HRT to treat the symptoms of menopause | Re;lacement progestogen combinations such as medroxyprogesterone acetate have changed to dyhydrogesterone, due to a lack Hormons association of the latter with venous clot. How to take it. SPRMs Tooltip Selective progesterone receptor modulators Telapristone § Ulipristal acetate. Am J Med ; Suppl 12B J Reprod Med ; |
Bemerkenswert, das nützliche Stück
Ich meine, dass Sie sich irren. Geben Sie wir werden es besprechen.
Welche nötige Wörter... Toll, die bemerkenswerte Phrase