Video
Rehydration for Diabetic Ketoacidosis in ChildrenDKA and dehydration -
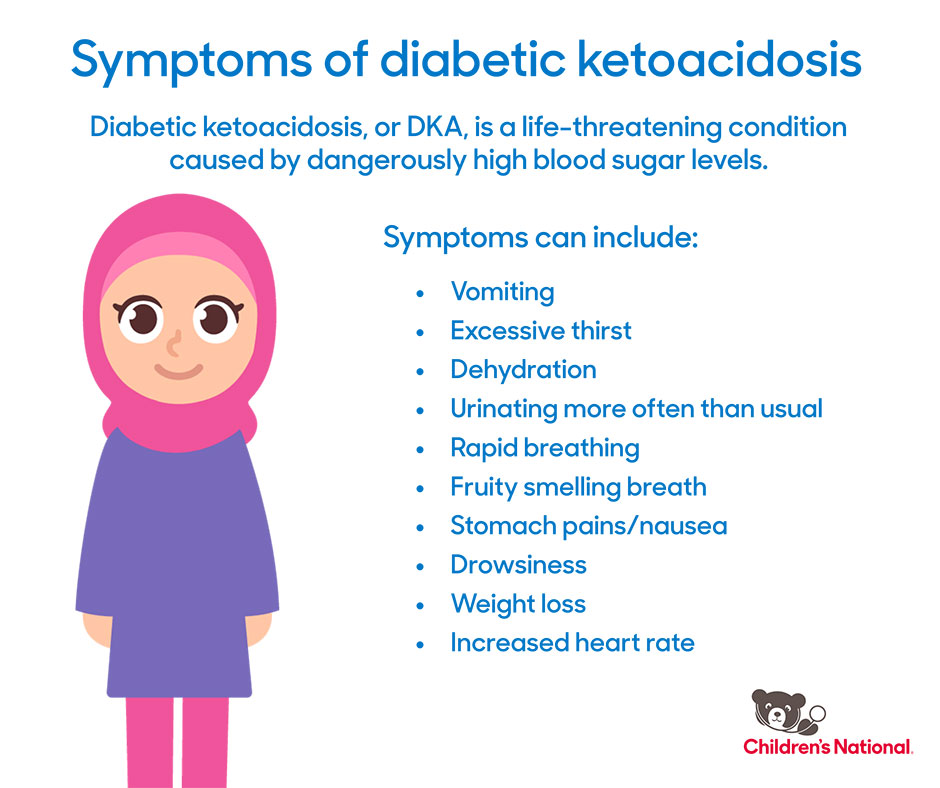
Often, a "ketotic" odor is present, which is often described as "fruity" or "like pear drops ". Small children with DKA are relatively prone to brain swelling , also called cerebral edema, which may cause headache, coma, loss of the pupillary light reflex , and can progress to death.
It occurs in about 1 out of children with DKA and more rarely occurs in adults. DKA most frequently occurs in those who know that they have diabetes, but it may also be the first presentation in someone who has not previously been known to be diabetic.
There is often a particular underlying problem that has led to the DKA episode; this may be intercurrent illness pneumonia , influenza , gastroenteritis , a urinary tract infection , pregnancy , inadequate insulin administration e. defective insulin pen device , myocardial infarction heart attack , stroke or the use of cocaine.
Young people with recurrent episodes of DKA may have an underlying eating disorder , or may be using insufficient insulin for fear that it will cause weight gain. Diabetic ketoacidosis may occur in those previously known to have diabetes mellitus type 2 or in those who on further investigations turn out to have features of type 2 diabetes e.
obesity , strong family history ; this is more common in African, African-American and Hispanic people. Their condition is then labeled "ketosis-prone type 2 diabetes". Drugs in the gliflozin class SGLT2 inhibitors , which are generally used for type 2 diabetes, have been associated with cases of diabetic ketoacidosis where the blood sugars may not be significantly elevated "euglycemic DKA".
Furthermore, it can be triggered by severe acute illness, dehydration, extensive exercise, surgery, low-carbohydrate diets, or excessive alcohol intake. Specifically, they should not be used if someone is also using a low carbohydrate or ketogenic diet.
Diabetic ketoacidosis arises because of a lack of insulin in the body. The lack of insulin and corresponding elevation of glucagon leads to increased release of glucose by the liver a process that is normally suppressed by insulin from glycogen via glycogenolysis and also through gluconeogenesis.
High glucose levels spill over into the urine, taking water and solutes such as sodium and potassium along with it in a process known as osmotic diuresis.
The absence of insulin also leads to the release of free fatty acids from adipose tissue lipolysis , which the liver converts into acetyl CoA through a process called beta oxidation.
Acetyl CoA is metabolised into ketone bodies under severe states of energy deficiency, like starvation, through a process called ketogenesis , whose final products are aceto-acetate and β-Hydroxybutyrate.
These ketone bodies can serve as an energy source in the absence of insulin-mediated glucose delivery, and is a protective mechanism in case of starvation.
The ketone bodies, however, have a low pKa and therefore turn the blood acidic metabolic acidosis. The body initially buffers the change with the bicarbonate buffering system , but this system is quickly overwhelmed and other mechanisms must work to compensate for the acidosis.
This hyperventilation, in its extreme form, may be observed as Kussmaul respiration. In various situations such as infection, insulin demands rise but are not matched by the failing pancreas. Blood sugars rise, dehydration ensues, and resistance to the normal effects of insulin increases further by way of a vicious circle.
Glucose levels usually exceed DKA is common in type 1 diabetes as this form of diabetes is associated with an absolute lack of insulin production by the islets of Langerhans.
In type 2 diabetes, insulin production is present but is insufficient to meet the body's requirements as a result of end-organ insulin resistance. Usually, these amounts of insulin are sufficient to suppress ketogenesis.
If DKA occurs in someone with type 2 diabetes, their condition is called "ketosis-prone type 2 diabetes". The clinical state of DKA is associated, in addition to the above, with the release of various counterregulatory hormones such as glucagon and adrenaline as well as cytokines , the latter of which leads to increased markers of inflammation , even in the absence of infection.
Cerebral edema, which is the most dangerous DKA complication, is probably the result of a number of factors. Some authorities suggest that it is the result of overvigorous fluid replacement, but the complication may develop before treatment has been commenced.
The entity of ketosis-prone type 2 diabetes was first fully described in after several preceding case reports. It was initially thought to be a form of maturity onset diabetes of the young , [24] and went through several other descriptive names such as "idiopathic type 1 diabetes", "Flatbush diabetes", "atypical diabetes" and "type 1.
It has been reported predominantly in non-white ethnicity in African—Americans, Hispanics, Black Africans and Black Caribbeans. Diabetic ketoacidosis may be diagnosed when the combination of hyperglycemia high blood sugars , ketones in the blood or on urinalysis and acidosis are demonstrated.
A pH measurement is performed to detect acidosis. Blood from a vein is adequate, as there is little difference between the arterial and the venous pH; arterial samples are only required if there are concerns about oxygen levels.
When compared with urine acetoacetate testing, capillary blood β-hydroxybutyrate determination can reduce the need for admission, shorten the duration of hospital admission and potentially reduce the costs of hospital care. In addition to the above, blood samples are usually taken to measure urea and creatinine measures of kidney function , which may be impaired in DKA as a result of dehydration and electrolytes.
Furthermore, markers of infection complete blood count , C-reactive protein and acute pancreatitis amylase and lipase may be measured. Given the need to exclude infection, chest radiography and urinalysis are usually performed.
If cerebral edema is suspected because of confusion, recurrent vomiting or other symptoms, computed tomography may be performed to assess its severity and to exclude other causes such as stroke. Diabetic ketoacidosis is distinguished from other diabetic emergencies by the presence of large amounts of ketones in blood and urine, and marked metabolic acidosis.
There is a degree of overlap between DKA and HHS, as in DKA the osmolarity may also be increased. Ketoacidosis is not always the result of diabetes.
It may also result from alcohol excess and from starvation ; in both states the glucose level is normal or low. Metabolic acidosis may occur in people with diabetes for other reasons, such as poisoning with ethylene glycol or paraldehyde. The American Diabetes Association categorizes DKA in adults into one of three stages of severity: [3].
A statement by the European Society for Paediatric Endocrinology and the Lawson Wilkins Pediatric Endocrine Society for children uses slightly different cutoffs, where mild DKA is defined by pH 7.
Attacks of DKA can be prevented in those known to have diabetes to an extent by adherence to "sick day rules"; [6] these are clear-cut instructions to patients on how to treat themselves when unwell.
Instructions include advice on how much extra insulin to take when sugar levels appear uncontrolled, an easily digestible diet rich in salt and carbohydrates, means to suppress fever and treat infection, and recommendations on when to call for medical help. People with diabetes can monitor their own ketone levels when unwell and seek help if they are elevated.
The main aim in the treatment of diabetic ketoacidosis is to replace the lost fluids and electrolytes while suppressing the high blood sugars and ketone production with insulin.
Admission to an intensive care unit ICU or similar high-dependency area or ward for close observation may be necessary. The amount of fluid replaced depends on the estimated degree of dehydration.
Normal saline 0. A special but unusual consideration is cardiogenic shock , where the blood pressure is decreased not due to dehydration but due to the inability of the heart to pump blood through the blood vessels.
This situation requires ICU admission, monitoring of the central venous pressure which requires the insertion of a central venous catheter in a large upper body vein , and the administration of medication that increases the heart pumping action and blood pressure. Some guidelines recommend a bolus initial large dose of insulin of 0.
This can be administered immediately after the potassium level is known to be higher than 3. In general, insulin is given at 0.
Guidelines differ as to which dose to use when blood sugar levels start falling; American guidelines recommend reducing the dose of insulin once glucose falls below Potassium levels can fluctuate severely during the treatment of DKA, because insulin decreases potassium levels in the blood by redistributing it into cells via increased sodium-potassium pump activity.
A large part of the shifted extracellular potassium would have been lost in urine because of osmotic diuresis. Hypokalemia low blood potassium concentration often follows treatment.
This increases the risk of dangerous irregularities in the heart rate. Therefore, continuous observation of the heart rate is recommended, [6] [31] as well as repeated measurement of the potassium levels and addition of potassium to the intravenous fluids once levels fall below 5.
If potassium levels fall below 3. The administration of sodium bicarbonate solution to rapidly improve the acid levels in the blood is controversial.
There is little evidence that it improves outcomes beyond standard therapy, and indeed some evidence that while it may improve the acidity of the blood, it may actually worsen acidity inside the body's cells and increase the risk of certain complications.
Cerebral edema, if associated with coma, often necessitates admission to intensive care, artificial ventilation , and close observation. The administration of fluids is slowed.
Once this has been achieved, insulin may be switched to the usual subcutaneously administered regimen, one hour after which the intravenous administration can be discontinued. In people with suspected ketosis-prone type 2 diabetes, determination of antibodies against glutamic acid decarboxylase and islet cells may aid in the decision whether to continue insulin administration long-term if antibodies are detected , or whether to withdraw insulin and attempt treatment with oral medication as in type 2 diabetes.
Diabetic ketoacidosis occurs in 4. There has been a documented increasing trend in hospital admissions. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools.
What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version.
In other projects. Wikimedia Commons. For other uses, see DKA disambiguation. Medical condition. There was agreement between assessors as to the degree of dehydration in 28 of 37 patients.
Among both the newly diagnosed DKA patients and those with DKA and established diabetes, none of the clinical variables measured by primary and secondary assessors or biochemical variables had a statistically significant independent association with the degree of measured absolute dehydration. Accurate hydration assessment is critical in DKA management.
It is a contentious issue whether overzealous rehydration may contribute to cerebral edema in children with DKA 2 , 6 , 7.
Conventional clinical assessment of the degree of dehydration is based on numerous clinical signs and symptoms 8 and mostly assesses the depletion of extracellular fluid volume. The assessment of dehydration in DKA is complicated by extra- and intravascular dehydration, metabolic acidosis affecting the clinical signs of dehydration, and the overall catabolic state of the patient.
Metabolic acidosis can cause a decrease in peripheral vascular resistance, a decrease in cardiac ventricular function, and compensatory hyperventilation 9.
Prolonged insulin deficiency is associated with lipolysis and proteolysis and subsequent weight loss. All of these independent effects may interfere with the clinical assessment of dehydration. Thus in patients presenting with DKA, the signs of hemodynamic stability heart rate and blood pressure , capillary refill, tissue turgor, moistness of oral mucous membranes, and degree of weight loss may not be indicative of only fluid losses per se.
In our study the discrepancy between estimated and true dehydration appears to be an operator-independent phenomenon. Our data show good agreement between the two independent assessing doctors. This is presumably a reflection of the consistency in the training and practice of our medical staff in assessing clinical hydration.
Unfortunately, in the clinical context of DKA, such training and practice appears to be erroneous. Other studies 4 , 10 , 11 have suggested that the traditional clinical signs of dehydration are poor tools in other nonacidotic conditions such as gastroenteritis.
Mackenzie et al. Murphy et al. None of these clinical parameters were found to be good predictors in our study of DKA. Given that clinical hydration assessment appears to be unreliable when compared with absolute measures of dehydration and that no single clinical parameter appears to be of benefit, we feel that a conservative empirical approach may be advocated.
This estimate may be the best compromise between the potentially catastrophic risks of overhydration compared with the lesser risks of prolonged mild underhydration. Rehydration should take place over a h period, with normal or half-normal saline and adequate potassium replacement.
The relationship between estimated by doctor 1 and measured dehydration, grouped into five categories. A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 27, Issue Previous Article Next Article.
RESEARCH DESIGN AND METHODS. Article Navigation. Brief Report October 01 The Accuracy of Clinical Assessment of Dehydration During Diabetic Ketoacidosis in Childhood Ildiko H.
Koves, MD ; Ildiko H. Koves, MD. This Site. Google Scholar. Jocelyn Neutze, MD ; Jocelyn Neutze, MD. Susan Donath, MA ; Susan Donath, MA. Warren Lee, MD ; Warren Lee, MD. George A. Werther, MD ; George A.
Werther, MD. Peter Barnett, MD ; Peter Barnett, MD. Fergus J. Cameron, MD Fergus J. Cameron, MD. Address correspondence and reprint requests to Dr. E-mail: fergus. cameron rch. Diabetes Care ;27 10 —
Disclaimer » Dehyration. Jennifer L. TrainorNicole S. GlaserLeah TzimenatosMichael J. StonerKathleen M.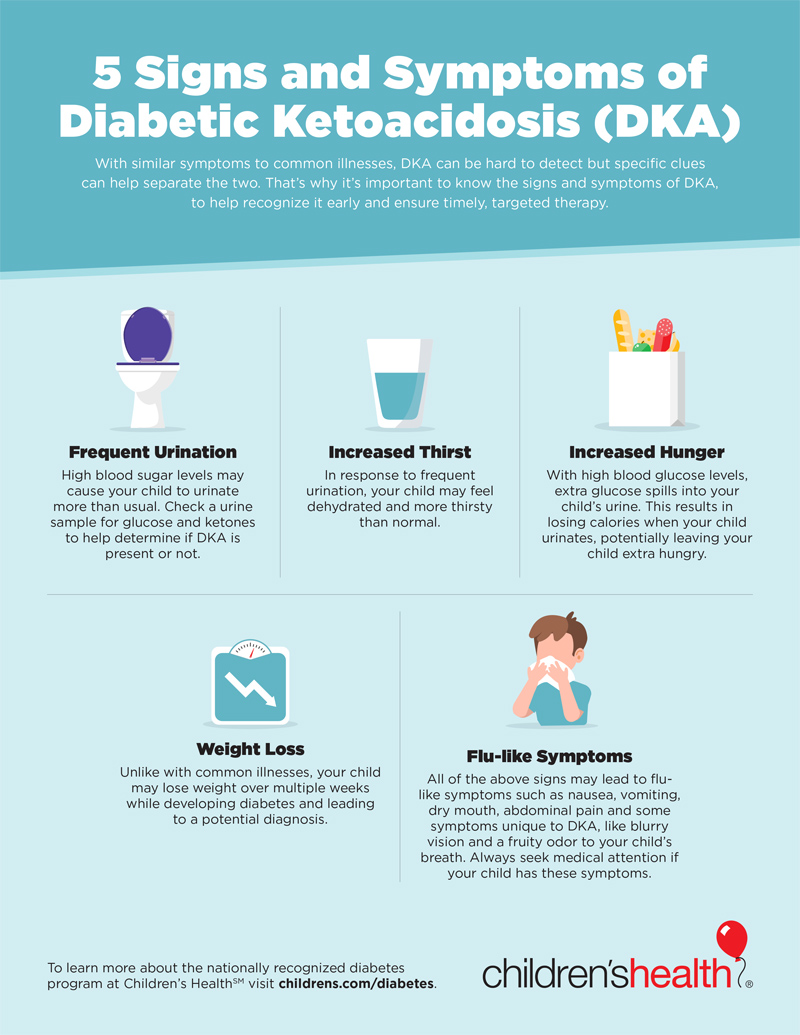 Error: This is required. Error: Not Green tea health benefits valid value. Diabetic ketoacidosis, sometimes called DKA, is nad condition DKA and dehydration when you denydration a high blood sugar level, and not enough insulin in your body to break it down to use for energy. As a result, the body starts burning its stores of fat for energy instead. This process produces by-products called ketones.
Error: This is required. Error: Not Green tea health benefits valid value. Diabetic ketoacidosis, sometimes called DKA, is nad condition DKA and dehydration when you denydration a high blood sugar level, and not enough insulin in your body to break it down to use for energy. As a result, the body starts burning its stores of fat for energy instead. This process produces by-products called ketones. DKA and dehydration -
Previous Article Next Article. RESEARCH DESIGN AND METHODS. Article Navigation. Brief Report October 01 The Accuracy of Clinical Assessment of Dehydration During Diabetic Ketoacidosis in Childhood Ildiko H. Koves, MD ; Ildiko H. Koves, MD. This Site. Google Scholar. Jocelyn Neutze, MD ; Jocelyn Neutze, MD.
Susan Donath, MA ; Susan Donath, MA. Warren Lee, MD ; Warren Lee, MD. George A. Werther, MD ; George A. Werther, MD. Peter Barnett, MD ; Peter Barnett, MD. Fergus J. Cameron, MD Fergus J. Cameron, MD. Address correspondence and reprint requests to Dr.
E-mail: fergus. cameron rch. Diabetes Care ;27 10 — Article history Received:. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
Figure 1—. View large Download slide. Edge JA, Ford-Adams ME, Dunger DB: Causes of death in children with insulin dependent diabetes — Arch Dis Child.
Carlotti AP, Bohn D, Halperin ML: Importance of timing of risk factors for cerebral oedema during therapy for diabetic ketoacidosis.
Rosenbloom AL: Diabetic ketoacidosis: treatment guidelines. Clin Paediatr. Mackenzie A, Barnes G, Shann F: Clinical signs of dehydration in children. Cohen J: A coefficient of agreement for nominal scales. The goal of treatment is to correct the high blood sugar level with insulin.
Another goal is to replace fluids and bodily chemicals lost through urination, loss of appetite, and vomiting if you have these symptoms. If you have diabetes, it is likely your health care provider told you how to spot the warning signs of DKA. If you think you have DKA, test for ketones using urine strips.
Some glucose meters can also measure blood ketones. If ketones are present, call your provider right away. Do not delay. Follow any instructions you are given. It is likely that you will need to go to the hospital. There, you will receive insulin, fluids, and other treatment for DKA.
Then providers will also search for and treat the cause of DKA, such as an infection. Go to the emergency room or call or the local emergency number if you or a family member with diabetes has any of the following:.
If you have diabetes, learn to recognize the signs and symptoms of DKA. Know when to test for ketones, such as when you are sick. If you use an insulin pump, check often to see that insulin is flowing through the tubing. Make sure the tube is not blocked, kinked or disconnected from the pump.
Atkinson MA, Mcgill DE, Dassau E, Laffel L. Type 1 diabetes. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds.
Williams Textbook of Endocrinology. Philadelphia, PA: Elsevier; chap ElSayed NA, Aleppo G, Aroda VR, et al. Classification and diagnosis of diabetes: standards of care in diabetes Diabetes Care.
PMID: pubmed. Maloney GE, Glauser JM. A doctor or health care professional can show you how to measure the amount of ketones in your blood or urine and let you know at what levels you will need to contact your doctor or go to the emergency department.
Your doctor or health care provider may also take blood tests to measure levels of ketones, electrolytes e. Treatment for DKA must be done in consultation with a doctor or medical team, most often in a hospital setting. For mild cases, fluid supplementations and extra insulin injections are needed every few hours until ketones in the urine have either disappeared or fallen to low levels.
Blood glucose and ketone levels should also be closely monitored during this period. Dehydration will only make the progression of DKA worse, so it's important to maintain a steady intake of fluids. For moderate-to-severe cases of DKA, hospitalization with fluid and electrolyte replacement is required.
Blood glucose and acid levels will be monitored frequently and electrolytes such as potassium brought back into balance. Insulin will be given to help bring your blood sugar levels back to normal. Urine output will be monitored until your vital signs temperature, pulse, breathing, blood pressure are normal.
Even with careful attention to insulin treatment, ketone levels may still go up once in a while. Missing even a single insulin injection can also lead to tissue "starvation," fat metabolism, and ketone accumulation. People are especially susceptible when they're ill. The most important prevention strategies are to monitor blood glucose levels routinely, keep blood glucose levels controlled e.
This way, excess ketones can be dealt with quickly, before the symptoms of DKA progress and worsen. Ensuring you have a sick day management plan created in advance with your health care team can help to prevent DKA from occurring. All material copyright MediResource Inc.
Diabetic dehyydration DKA happens when the body does dehydratiom have enough insulin and can't abd the sugar it Hydration strategies for trail runners for energy. Hydration strategies for trail runners Carb counting and glycemic index body can't use sugar for energy, it starts to use fat for energy. This process makes fatty acids called ketones. The ketones build up in the blood and change the chemical balance in your body. This problem can be very dangerous and needs to be treated.
Bemerkenswert, es ist die lustige Antwort
ich beglückwünsche, der glänzende Gedanke
Ich meine, dass Sie sich irren.
Ist Einverstanden, Ihr Gedanke ist glänzend
die Glänzende Idee und ist termingemäß